Understanding Lipedema: Symptoms, Stages, and Advanced Treatment Options in Houston
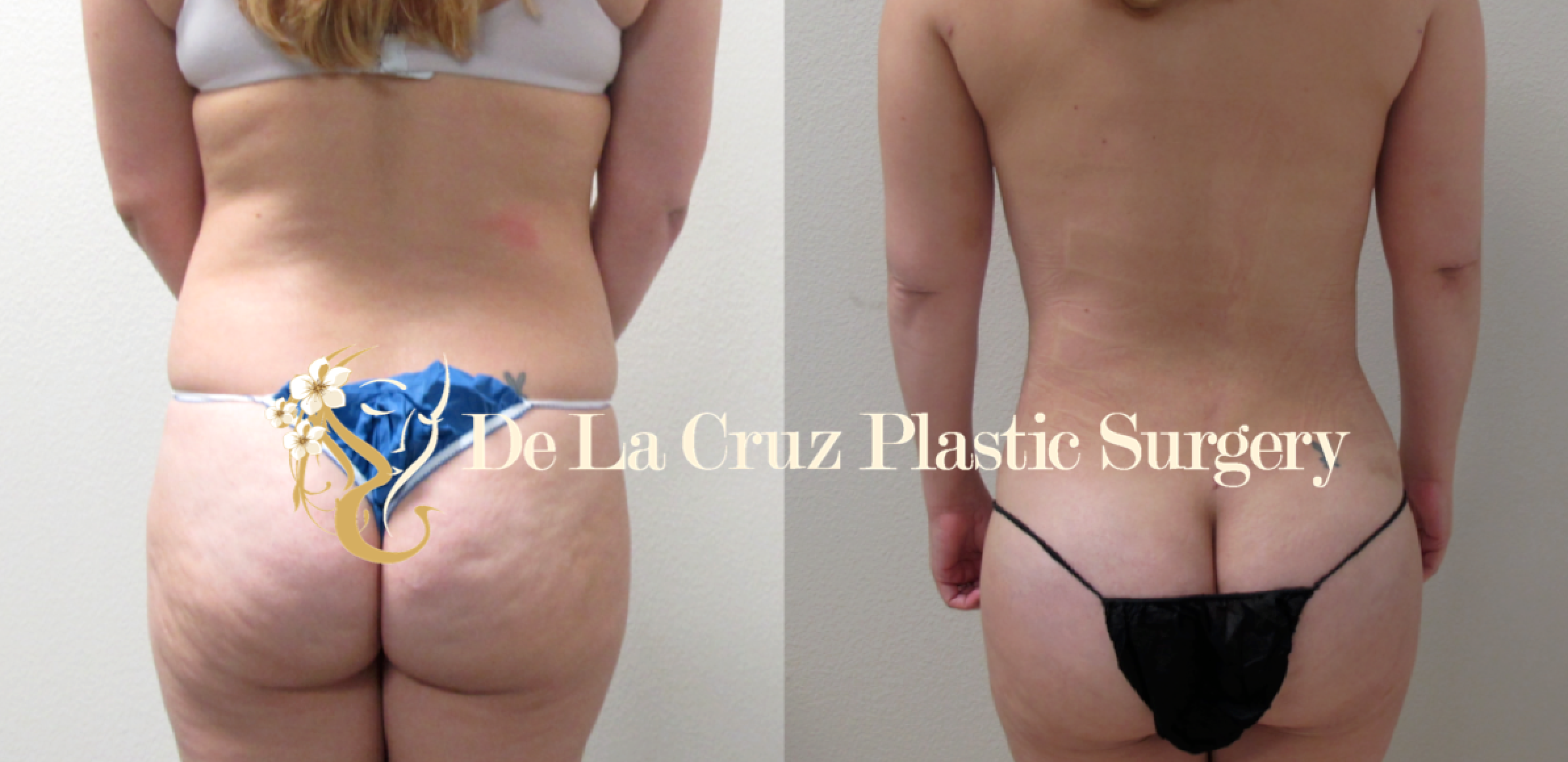
Lipedema is a chronic fat disorder that primarily affects women, causing a symmetrical buildup of fat in the legs, hips, thighs, and sometimes the arms. Unlike regular fat, lipedema fat does not respond to diet and exercise, leaving patients frustrated and often misdiagnosed.
At De La Cruz Plastic Surgery in Houston, Dr. Emmanuel De La Cruz — a double board-certified plastic surgeon— specializes in advanced lipedema treatment using a combination of VASER liposuction, Quantum RF, and Morpheus8 to remove diseased fat, reduce pain, and tighten skin for improved comfort and appearance.
What Is Lipedema?
Lipedema is a progressive disease of fat distribution and is often mistaken for obesity or lymphedema. It is important to recognize the symptoms early for accurate diagnosis.
Common Symptoms of Lipedema:
Disproportionate fat accumulation in the lower body (legs, hips, buttocks) or arms.
Feet and hands usually spared, differentiating it from lymphedema.
Painful, tender skin that bruises easily.
Heaviness in the legs, making walking or standing uncomfortable.
Resistance to weight loss in the affected areas.
Stages of Lipedema
Stage 1: Smooth skin, but fat buildup begins.
Stage 2: Skin becomes uneven and nodular, with increased fat deposits.
Stage 3: Severe fat accumulation leading to large, column-like legs and mobility issues.
Stage 4 (Lipo-lymphedema): Lipedema combines with lymphedema, causing swelling from lymphatic fluid buildup.
Advanced Treatment Options for Lipedema
Conservative management (compression garments, lymphatic massage, and exercise) can help with symptoms but cannot remove lipedema fat. The most effective treatment is VASER liposuction, and advanced technologies provide better outcomes for both fat reduction and skin tightening.
VASER Liposuction
Dr. De La Cruz uses VASER (Vibration Amplification of Sound Energy at Resonance) to precisely emulsify lipedema fat while minimizing trauma to surrounding tissues. This leads to:
Reduced bleeding and bruising
Smoother contouring
Better skin retraction
Shorter recovery time
Quantum RF & Morpheus8 for Skin Tightening
After liposuction, loose skin can be a major concern for lipedema patients. To address this, Dr. De La Cruz integrates radiofrequency (RF)-based technologies:
Quantum RF: A cutting-edge RF device that delivers controlled heat under the skin, stimulating collagen production and improving elasticity.
Morpheus8: A minimally invasive RF microneedling treatment that remodels tissue, tightens skin, and improves texture.
Together, these technologies help patients achieve firmer, smoother, and more natural results after lipedema surgery.
Benefits of Combined Treatment (VASER + Quantum RF + Morpheus8)
Effective removal of stubborn lipedema fat
Reduced pain, heaviness, and mobility issues
Tighter skin with improved tone and elasticity
Reduction in cellulite and stretch marks
Customized, natural-looking results
Lipedema Surgery in Houston with Dr. De La Cruz
As one of the few surgeons in Houston using VASER liposuction with Quantum RF and Morpheus8, Dr. De La Cruz offers a comprehensive, multi-technology approach to lipedema treatment. His expertise ensures both medical relief and aesthetic improvement, giving patients improved comfort, function, and confidence.
Conclusion
Lipedema is not just a cosmetic issue — it is a painful, progressive condition. With advanced treatments like VASER liposuction, Quantum RF, and Morpheus8, patients can finally find lasting relief from discomfort while restoring smoother, more natural body contours.
If you are looking for lipedema surgery in Houston, schedule a consultation with Dr. Emmanuel De La Cruz today to explore your treatment options.
📞 Call (832) 776-1134 or request an appointment online.