Potential Complications of a Tummy Tuck Procedure (Abdominoplasty)
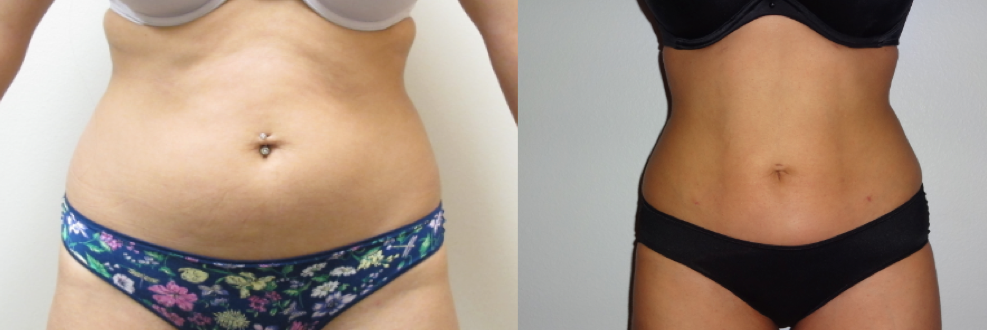
One of the most common cosmetic surgeries patients are interested in when they come to my office is the abdominoplasty. This procedure, generally known as tummy tuck, can flatten your abdomen by removing loose, excess fat and skin and tightening muscles in the abdominal wall. One benefit that patients appreciate the most is that it can also remove the stretch marks in your lower abdomen. It is popular following pregnancy, massive weight loss or whenever a saggy abdomen with weak muscles impairs body contour.
When performed by an experienced board certified plastic surgeon, the abdominoplasty will result in flatter, firmer abdominal contour with narrower waistline that wouldn’t be achieved by liposuction procedures only. All in all, abdominoplasty is a very safe operation. Unfortunately, as with any other cosmetic surgeries, there are post-operative complications that should be addressed by a specialist in a time manner. The most likely possible complications after abdominoplasty are: swelling, infection, wound separation and fluid collections (seromas and hematomas).
The swelling is manifested in the upper thighs and in some cases in the lower legs. The abdominal skin flap can stay swollen due to lymphatic blockage weeks after surgery. This type of swelling requires compression, because swollen tissues themselves can cause more scarring. To prevent the swelling that can occur following a tummy tuck procedure, I prefer the Lockwood technique because separates less tissues than the standard technique. Moreover, one significant thing you can do to control the swelling after the surgery is to wear the post-op compression garment 24/7 for at least eight weeks. Have in mind that tissues heal better and faster when there is minimal swelling.
Infection is another possible complication that can occur after abdominoplasty. Usually, I prescribe patients antibiotics during their final pre-operative visit to prevent wound infection. It is important that patients make sure they are not allergic to the antibiotics prescribed by their surgeons. Oral temperature over 100.4 degrees, yellowish or greenish drainage from the incisions and/or foul odor are among the indicators of a possible infection. A suture abscess is typically not dangerous and it’s easily taken care of by lancing the area under a local anesthetic, and packing the small puncture with a medicated gauze. However, infections can also be life threatening, like those of MRSA (Methicillin Resistant Staph Aureus). It’s always best for patients to contact their doctor promptly if they have any sign of infection. Therefore, I facilitate my cell phone number to all of my post-op patients so they can communicate immediately if any problems or concerns arise.
Wound separation can also be a possible complication after an abdominoplasty. Excess skin tension if too much skin was taking out during the procedure can cause the wound to separate. Small wound separations are easily taken care of by packing the wound with medicated gauze. Slightly larger wound separations can be taken care of by a suction device called a “Vac Dressing”. Large wound separations caused by poor blood supply may need revision and re-approximation of the wound edges in a procedure room.
In any case, I highly recommend patients to schedule an in-person visit to get the wound treated promptly and prevent further complications such as getting the wound infected or extending the recovery period.
Lastly, fluid collections (namely seromas and hematomas) are among the possible complications after a tummy tuck procedure. A seroma is a collection of wound fluid. Sometimes it occurs when patients do not wear the compression garment adequately or he/she has a lot of activity in the post-operative period. For its part, a hematoma is a collection of blood in the dead space. It usually needs to be evacuated because it can be painful, can lead to infection or cause excessive scarring. Although seromas and hematomas can be easily treated with a needle aspiration, the best remedy against fluid collections is prevention. The proper use of compression garments and foam pads (Topifoam pads) over areas of potential fluid accumulation are significantly beneficial to prevent these post-operative complications.